Proficiency based progression training for epidural catheter placement for labour analgesia
Medical errors account for as many as 250,000 deaths in the US every year. A significant proportion of such errors (44% by one estimate) are related to procedural skills. Although simulation based training methods have been developed to address the deficiencies in training, there is limited evidence to show it reduces procedural errors or that it improves patient outcomes. By employing a tool known as “Proficiency-based progression (PBP)” we were able to show improved patient outcomes. Previous investigations of medical training using this tool have focused on the performance of the doctor rather than a meaningful patient outcome.
This study titled “Proficiency-based progression training: an “end to end” model for decreasing error applied to achievement of effective epidural analgesia during labour -a randomized control study” was published in the British Medical Journal Open (BMJ Open). In developing the training technique, we selected a procedure—in this case epidural—and broken it down into a series of “microtasks”or “Metrics”. We observed both experts and novices in epidural catheter insertion performing each microtask with the focus on what should or should not happen, and at the end of an eight-month process, a series of metrics emerged.
Anaesthesia trainees had to successfully demonstrate their competence in each metric — 74 in all — before progressing to the next step or microtask. For instance, one metric required the doctor to cover an A4-sized area of the patient’s back when painting on aseptic solution. In the event of not meeting this requirement, they were deemed not to have completed the metric. Training could not progress until the metric was met.
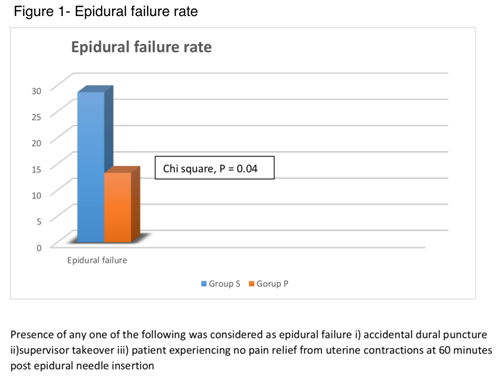
This training tool that could measure the trainee’s effectiveness along each tiny step of a procedure proved highly effective in our trial. In fact patients of trainees who had trained using this tool responded much more positively to epidural compared to doctors who underwent standard simulation based training. The failure rate for those with standard training was 24% compared to 12% who used the PBP effectively halving the failure rate (figure 1).
One hundred and 40 women took part in the clinical trial at CUMH between January 2015 and September 2016. To be eligible, it had to be established that they were in labour and had chosen to have an epidural. If the midwife deemed the patient to be comfortable within 60 minutes or less of having the epidural, the procedure was deemed a success.
The limitations of the trial were the small sample size and the fact that it took place in just one hospital. However this study assumes importance in that it is the first of its kind where a training modality has shown to improve patient outcomes in a meaningful manner.