Projects
Projects
Helping Babies Breathe (HBB)
In January 2013, Prof. Tony Ryan, Consultant Neonatologist, Cork University Maternity Hospital (CUMH) and Dr Sami Ahmed, Consultant Paeditrician, Bons Secours Hospital, Cork spent a week delivering the Helping Babies Breathe (HBB) in Northern Sudan. Helping Babies Breathe is a neonatal resuscitation curriculum for resource-limited circumstances. It was developed on the premise that assessment at birth and simple newborn care are things that every baby deserves. The initial steps taught in HBB can save lives and give a much better start to many babies who struggle to breathe at birth. The focus is to meet the needs of every baby born.
The HBB training programme was delivered to 80 paediatricians and senior health midwives from across Northern Sudan who in turn will train hundreds of village midwives on neonatal resuscitation. This national Train the Trainer programme was sponsored by Irish Aid (http://www.irishaid.ie/), Department of Foreign Affairs and Trade, and supported by the State and Federal Ministries of Health in Northern Sudan to reduce infant mortality by building the knowledge and skills of healthcare professionals.
HBB, a programme designed by the American Academy of Paediatrics, was delivered at the Continuing Professional Development Directorate (CPDD) in conjunction with;
- Prof Anthony Ryan, Consultant Neonatologist, Cork University Maternity Hospital, Cork, Ireland.
- Dr Sami Ahmed, Consultant Paediatrician, Bons Secours Hospital, Cork, Ireland.
- Dr Abdel Moniem Hamid, Consultant Paediatrician, Khartoum General Hospital, Sudan.
- Prof George A. Little, Co-Chairperson of the HBB Global Implementation Task Force, Department of Paediatrics, Children’s Hospital, Dartmouth-Hitchcock Medical Centre, Lebanon, New Hampshire, USA.
- Dr Carol Little, Department of Paediatrics, Children’s Hospital, Dartmouth-Hitchcock Medical Centre, Lebanon, New Hampshire, USA.
- Dr Lisa Clark, Paediatric Nurse Practitioner at Stony Brook Long Island Children’s Hospital, USA.
- Victoria Flanagan, RN, MS, Regional Program for Women’s and Children’s Health, Dartmouth-Hitchcock Medical Centre, USA.

The implementation of HBB has continued in Northern Sudan in each of the 22 regional training centres since the initial Master Trainer HBB programme in January 2013. Over 1,000 bag and masks, and training equipment have been provided to midwives in the regions listed below. The following areas have since received registered Helping Babies Breathe training programmes.
| Date | State | Town | No. of Candidates (Midwives) | No. of Certified Midwives | Cumulative Total |
| 27th - 28th January | Gazira | Barakat | 22 | 22 | 22 |
| 11th-12th February | North Korodofan | Umrawaba | 22 | 22 | 44 |
| 17th - 18th February | North Korodofan | Abuzabad | 31 | 31 | 75 |
| 19th February | North Korodofan | Jabrat Alsheikh | 26 | 26 | 101 |
| 19th February | North Korodofan | Umdam | 25 | 25 | 126 |
| 19th February | North Korodofan | Alidhaya | 32 | 32 | 158 |
| 19th February | North Korodofan | Wadbanda/Gibesh/Alnuhud | 33 | 33 | 191 |
| 19th February | North Korodofan | Bara West | 31 | 31 | 222 |
| 19th February | North Korodofan | Sodary | 31 | 31 | 253 |
| 8th - 9th May | Kassala | Kassala | 20 | 20 | 273 |
| 10th - 11th May | Kassala | Kassala | 20 | 20 | 293 |
| 10th - 11th June | Gedarif | Gedarif | 18 | 18 | 311 |
| 12th - 13th June | Gedarif | Gedarif | 18 | 18 | 329 |
| 15th - 16th June | North Darfur | Alfashir | 21 | 21 | 350 |
| 25th - 26th June | North Darfur | Alfashir | 20 | 20 | 370 |
| 7th - 8th July | Khartoum | Khartoum North | 22 | 22 | 392 |
| 7th - 8th July | Khartoum | Omdurman Maternity | 46 | 46 | 438 |
| 19th - 20th July | North Darfur | Saraf Amra | 22 | 22 | 460 |
| 18th - 19th September | North Darfur | Kabkabia | 21 | 21 | 481 |
| 19th - 20th September | North Darfur | Daralsalam | 21 | 21 | 502 |
| 20th - 21st September | North Darfur | Alfashir | 21 | 21 | 523 |
| 23rd - 24th September | Red Sea | Port Sudan | 21 | 21 | 544 |
| 27th - 28th September | Kassala | Kassala | 20 | 20 | 564 |
| 29th - 30th September | Kassala | Kassala | 30 | 30 | 594 |
| 1st - 2nd October | Kassala | Kassala | 20 | 20 | 614 |
| Total 2013 | 614 |

As courses are on the increase, this necessitated increasing the number of trainers (currently 3 in each state- 2 health visitors plus a paediatrician). Two facilitator courses were run as follows:
1. One HBB facilitators (TOT) course was done at Alfashir, North Darfur upon the State request on 27th and 28th June 2013. Dr Ishag, Sister Hind and Dr. Abdelmoniem ran the course. 14 out of 20 health visitors were certified. This raised the number of Tutors in this state alone to 17.
2. Another TOT was held at CPD Khartoum. Two health visitors were selected from each of the 17 Sudan states. 38 candidates attended from 14 states. 32 candidates were certified as facilitators, 4 as providers and 2 did not get a satisfactory result.
This raises our trainer numbers from 85 in all states to 131. That means the traineres increased from 3-5 in each of the 22 centres in 14 Sudan states.
| Date | State | Town | No. of Candidates | No. of Certified Candidates | Cumulative Total |
| 15th - 16th January | Khartoum | Khartoum - CPD | 43 doctors and sister midwives | 43 | 43 |
| 17th - 18th January | Khartoum | Khartoum - CPD | 42 | 42 | 85 |
| 25th - 26th June | North Darfur | Alfashir | 20 | 14 | 99 |
| 5th - 6th July | Khartoum | Khartoum - CPD | 38 | 32 | 131 |
| Total | 131 |
The Helping Babies Breathe programme in Northern Sudan recently received €10,000 in funding from the Health Service Executive's (HSE) Staff of HSE (Cork and Kerry) Association for the Relief of Poverty (SHARP). This is a voluntary HSE employee contribution programme where staff members can donate a percentage of their salary to charitable causes. This grant will enable the HBB programme to train regional trainers across Northern Sudan so midwives at peripheral health centres, which can serve up to 50 villages, can be trained on HBB and receive the equipment they need, a bag and mask, for neonatal resuscitation.
More information on HBB can be found at the website: http://www.helpingbabiesbreathe.org/


eHealth Needs Analysis
Siobhán O’Connor, a mature student nurse at University College Cork with a background in information systems undertook a week long analysis of the information and communication technologies (ICT) in place at Omdurman Maternity Hospital, Northern Sudan. Ms O’Connor worked with Dr Murwan Omer, Clinical Director at Omdurman Maternity Hospital, along with his clinical and administrative teams to undertake a detailed computer system and business needs analysis at the maternity hospital.
She had several meetings and workshops throughout the week with key groups at Omdurman Maternity Hospital (OMH). As an example, Ms O’Connor met with Dr Atif Bashir Eltayeb Fazari, Consultant Obstetrician and Gynaecologist who leads the education and training of clinical staff and Ms Hana Awad, Library Manager at OMH. They discussed the setup of an e-learning hub in the hospital library to facilitate a series of online continuing professional development programmes between University College Cork and OMH. These would be essential in training junior doctors and midwives at OMH in specialised areas such as laparoscopic surgery and neonatal intensive care.

Ms O’Connor also met with Mr Omer Sirage Alnour, Deputy Director of IT and the staff of his department to discuss their training needs and the ICT infrastructure at the maternity hospital. It was clear that a robust IT network hindered the integration of clinical information systems they have developed for specific areas. The IT staff also lacked certain skills in database management, networking and web design to create more sophisticated computer systems for OMH. Ms O’Connor also met with Mr Ishag Ahmed and Sister Anyisha who together run the Statistics Department and are responsible for gathering and collating all the data on child births, antenatal clinics and admissions at Omdurman Maternity Hospital. They outlined the issues around data quality and data management at OMH due to the poor IT infrastructure and the need to build up the IT skills of clinical and administrative staff.

Ms O'Connor accompanied Prof. Anthony Ryan, Dr Sami Ahmed and others from Cork University Maternity Hospital, Ireland on a week long trip to Khartoum where a neonatal resuscitation programme called Helping Babies Breathe was taking place. The week long trip concluded on a high note with an awards ceremony at the Coral Hotel, Khartoum. Prof. Ryan and Dr. Ahmed were presented with awards by Prof. Mamoun Humaida, Minister of Health for Khartoum State for building up the Cork-Omdurman partnership over the last number of years and for their commitment to improving maternal and child health in Northern Sudan.
Ms Siobhán O’Connor along with Mr Yusuf Malik were also presented with gifts by Dr Murwan Omer for their contribution to education and research at Omdurman Maternity Hospital. The awards ceremony concluded with a civic reception and dinner attended by members of the Ministry of Health, the Sudanese Medical Council, the Sudan Association of Paediatricians and the Sudanese Society of Neonatologists.
Ms O’Connor is currently working with Prof. Ryan and her colleagues at University College Cork to further develop the ICT infrastructure at Omdurman Maternity Hospital and build the capacity of their own internal IT staff to learn new software skills and manage future eHealth projects.
Integrated Management of Childhood Illness (IMCI)
In developing countries, most of the 11 million deaths per year of children under the age five years occur in areas where adequate medical care is not available. In Sudan, Africa the under-five mortality rate is 133 per 1,000 live births. Malaria and infantile diarrhoea are two major causes of mortality in children under 5 years of age and other serious infections in this age group include pneumonia, measles and meningitis. Most child deaths could be avoided by prompt recognition and treatment.
The WHO and UNICEF developed the Integrated Management of Childhood Illness (IMCI) as a strategy to improve childhood survival and disease control. IMCI uses simple signs and symptoms to assess and classify illness, thus allowing community health workers at rural health clinics to identify which children have minor illnesses that need symptomatic treatment and urgent referral. However this paper based system has a number of limitations.

A mobile health project entitled "Supporting LIFE" is being coordinated and led by Dr John O'Donoghue and Dr Joe Gallahger, Directors of the Health Information Systems Research Centre (HISRC), University College Cork. Supporting LIFE is providing a low-cost, effective, targeted mobile health application called e-IMCI to improve child health assessment and disease management in low resource settings. It will also address inadequate healthcare disease reporting and surveillance infrastructures by providing district and zonal health officers as well as the Ministry of Health with real-time disease statistics through a mobile health information system. The e-IMCI application is been trialled in both Northern Sudan and Malawi in conjunction with local NGOs and national governments. Project website: http://www.supportinglife.eu/
Maternal Mortality
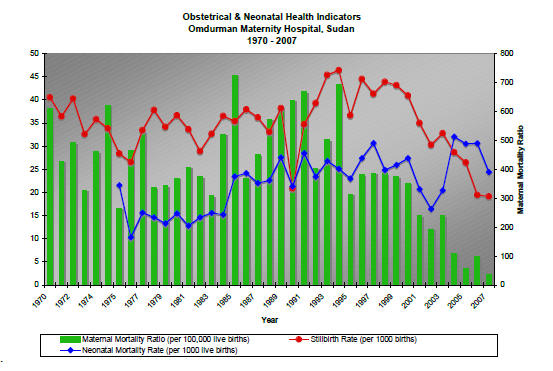
One of the major goals of the Cork University Maternity Hospital (CUMH) - Omdurman Maternity Hospital (OMH) Partnership was to implement evidence based and efficient obstetrics and gynaecological, neonatal and midwifery clinical practice to reduce maternal and perinatal mortality.
Cork city's three main maternity hospitals, the Erinville, St. Finbarr's and the Bons Secours hospital amalgamated into one large maternity hospital in 2007. During this process staff at the newly opened Cork University Maternity Hospital (CUMH) believed they had a valuable contribution in terms of human, financial, educational and organisational to offer a maternity hospital in a developing country. As CUMH prepared for the amalgamation of the three hospitals equipement such as beds, cots, incubators, warmers, ventilators, anaesthetic equipment were transferred to Omdurman Maternity Hospital, Northern Sudan. The cost of transporting this equipment to Sudan was supported through an Irish Aid grant which matched the value of the equipment being donated so a major capital investment could be made at OMH which also vastly improved infrastructure within the hospital. Additional fundraising was done and donations of baby clothes and medical books were made, and an ambulance was refitted by the Cork Fire Service for use in Sudan.

Evidence based measures have also been introduced over the last number of years due to continued training programmes which have helped reduce maternal mortality. These include initiatives such as the use of:
- Mg SO4 / Hydralazine for eclampsia
- Misoprostol for PPH
- Prophylactic antibiotics
- Thromboprophylaxis
- Guidelines and management protocols
- Audit and quality control
- Expansion / upgrade of antenatal care
- Continuous training
- 24 hr consultant cover on OMH site
There have also been improvements in Anaethetic services and Blood bank services which have contributed to a decline in maternal mortality.
Neonatal Resuscitation Programme (NRP)
A National Neonatal Resuscitation Programme (NRP) was esatblished in Khartoum University by Dr S. Ahmed, Prof I Salah and Prof Tony Ryan in 2002. Provider courses were followed up with NRP instructor courses to create a “cascade of teaching” by training local instructors: Subsequently, the multidisciplinary teams included Obstetricians, Midwives, Neonatal nurses, Paramedics, Respiratory specialists, and a hospital Administrator. There have been 10 multidisciplinary visits to Khartoum over the last decade (2002-2009) to run the NRP programme which have been supported by Irish Aid.



