News
News

European ESTHER Alliance meeting
Thursday 12th and Friday 13th December 2013 saw the gathering of ESTHER Alliance (http://www.esther.eu/) representatives from France, Germany, Greece, Ireland, Italy, Norway, Switzerland and the UK, at the Department of Foreign Affairs in Dublin, Ireland. Over the course of two days, the meeting’s attendees collaborated to help build the ESTHER Alliance’s coming 5-year strategy to strengthen institutional partnerships between European hospitals and health institutions, and their counterparts throughout countries in the developing world.

Friday morning’s proceedings were opened by Minister for Trade and Development, Joe Costello TD, who reaffirmed Ireland’s strong commitment to health systems strengthening overseas. This commitment was echoed by Dr Philip Crowley, National Director, Quality and Patient Safety of the Health Service Executive (HSE). Professor Tony Ryan of Cork University Maternity Hospital, which is partnered with Omdusman Maternity Hospital, Northern Sudan demonstrated the effectiveness of the Helping Babies Breathe (HBB) initiative which has been funded by both Irish Aid and the Health Service Executive's SHARP committee.

Other delegates spoke of their countries’ progress to-date, giving presentations on a wide range of novel and highly- useful initiatives, that have facilitated the international sharing of essential life-saving expertise, skills, personnel and resources. These partnerships have to-date made a significant difference in enhancing healthcare capacity in around 40 countries across sub-Saharan Africa, North Africa, Central and South America, and South-East Asia. The meeting helped further cement collaboration and knowledge-sharing between the ESTHER partners, to build best-practice, as well as facilitating strategic planning to help attain European Alliance goals, heading towards the post Millennium Development Goals period beyond 2015.

The Sudanese National Initiative - HBB
Helping Babies Breathe (HBB) project, a basic neonatal resuscitation training for Birth Attendants in resource limited countries, was implemented in Khartoum, Northern Sudan on 15th January 2013. Its main objective is to reduce neonatal mortality rate (NMR) estimated in Sudan as 35 per 1,000 newborn (2010). The initiative was supported by University College Cork (Ireland), Cork University Maternity Hospital (Ireland), the American Academy of Paediatrics (AAP), in addition to support and collaboration from The Federal Ministry of Health, Sudanese Neonatal and Sudanese Paediatric Associations. The initial phase of the programme was funded through Irish Aid and focused mainly on a cascade of training from Master trainers, Regional trainers, Midwifery trainers who taught Villiage Midwives from all of the 16 states in Sudan.
Seven Master Trainers from the USA (Prof George Little, Dr Carol Little, Dr Lisa Clark and Ms Victoria Flanagan), Ireland (Prof. Anthony Ryan) and Sudan (Dr Sami Ahmed, Dr Abdel Moniem Hamid) participated in the two facilitators/trainers courses organized at the (CPDC) in Khartoum 15-18th January 2013. With support from Irish Aid (http://www.dci.gov.ie/) and Sudan Federal & Local Ministries of Health, the program was developed for Master Trainer and Facilitator Trainer courses over 4 days for 30 physicians, 12 Sister midwives, and 42 health visitors who will then go out to train village midwives in 17 states and 23 CPD centers.
The Sudanese National Initiative - HBB
Since then the HBB project has progress significantly. Three candidates (Paediatrician & 2 Midwives/ Tutors) were chosen to represent each of 22 training centres over the country. HBB provider courses started first in the middle of January 2013, followed by West, East and South West of Sudan with 66 trainers returning back to their states after the courses, to start training more community midwives. The total number of midwives trained up until August 2013 was 239 and equipment for training an additional 750 midwives has since been forwarded to the CPDD in Khartoum, Northern Sudan. Another significnat achievement has been the incorporation of the HBB programme into the Midwifery Training Schools Curriculum by the National Academy, ensuring sustainability.
To speed up training, two more Train the Trainer courses were organized at Khartoum in July 2013, and 46 more midwives were trained, making a total of 131 facilitators in Northern Sudan. More funding is required to extend HBB training to all the VMWs in Sudan (about 14,000) over the next 4-5 yrs.
Federal Ministry of Health Sudan - HBB
Sudanese Association of Paediatrics - HBB
Sudanese Society of Neonatology - HBB
-575x431.jpg)
ESTHER Ireland
On June 26, 2013, Minister of State for Trade and Development Joe Costello TD launched the ESTHER Ireland programme beneath the stained glass windows of the Albert Hall, in the Royal College of Surgeons, Dublin. Ireland’s membership of ESTHER follows a Memorandum of Understanding signed between the Health Service Executive (HSE) and Irish Aid in 2010, in support of health needs in less developed countries, and Ireland joined the broader European ESTHER alliance in 2012. “This initiative will promote skill-sharing partnerships in countries with the greatest health needs," said Mr Costello. "We have a winner here with ESTHER – a new way of doing work”.
Mr Costello pointed out the impact of the two current ESTHER Ireland partnerships - Cork University Maternity Hospital (CUMH)-Omdurman Maternity Hospital (OMH) partnership and the RCSI and College of Surgeons of East, Central and Southern Africa (COSECSA) have collaboration. "We are already seeing very encouraging results: the partnership between Cork University Hospital and the Omdurman Maternity Hospital in Sudan is associated with an 86 per cent reduction in maternal mortality and a 50 per cent drop in stillbirths and early neonatal deaths," said Mr Costello.

“Partnerships such as these will contribute to major, sustainable improvement to health systems in those countries which are most vulnerable" he said. "They will also benefit Irish health professionals, who will gain invaluable experience and new skills. The Government’s new Policy on International Development commits us to harnessing the skills of Irish health experts and institutions to improve access to quality essential health services."
Also speaking at the launch were Dr David Weakliam, chair of ESTHER Ireland; Declan Magee, vice-president of RCSI; and Tony O'Brien, director general designate, HSE. According to Mr O'Brien, the benefits of the ESTHER Ireland programme will be felt on both sides - in Ireland and in partner countries. "The partnership approach means there are benefits on both sides, and the programme will contribute to improving quality of health care in Ireland as well as in the partner countries.”
Eric O'Fynn, programme manager of the RCSI-COSESCA collaboration, and Dr Sami Ahmed, of the CUMH-OMH partnership, were on hand to show the impact that their projects are already having on the ground, informing over 60 attendees about their projects.
Irish Aid Launches New Policy for International Development 2013
Irish Aid, Ireland's national development agency launched a new policy for International Develop in 2013. The policy document entitled "One World, One Future: Ireland’s Policy for International Development" sets out the vision, goals and priorities for the Government’s overseas aid programme over the coming four years, 2013 - 2017.
Irish Aid's policy can be downloaded here:
The Cork University Maternity Hospital (CUMH) - Omdurman Maternity Hospital (OMH) Partnership aligns directly with Irish Aid's new policies as it has a long track history of fostering sustainable healthcare initatives in Northern Sudan such as the Helping Babies Breathe (HBB) project and it has put in place structures which have embedded this neonatal resuscitation training programme into the national educational curriculum for community midwives. This will ensure HBB techniques continue long into the future.
The Cork University Maternity Hospital (CUMH) - Omdurman Maternity Hospital (OMH) Partnership also meets Irish Aid's requirements in terms of volunteerism as it has a strong track record of harnessing the experience of highly trained volunteers to bring substantial change in obstetric and gynaecological services in Northern Sudan. This includes many doctors, midwives, nurses, biomedical technicians, hospital administrators from Ireland's Health Service Executive (HSE) being involved in the partnership for training, education and research over the last 10 years. This has brought significant improvements in healthcare to Sudanese women with a new Fistula and Gynaecological Unit being opened in Omdurman Maternity Hospital in 2009.
The CUMH - OMH Partnership is committed to long term improvements in the health of newborns, infants and their mothers and has engaged effectively with the Federal Ministry of Health in Northern Sudan. The MOH have supported the Helping Babies Breathe (HBB) project through the Continuing Proefssional Development Directorate (CPDD) in Khartoum helping us to extend HBB to each of the 17 states in Sudan so thousands of community midwives all over Northern Sudan can be trained on this important life saving technique.
Finally in keeping with Irish Aid's requirement for openness, transparency and accountability a bi-lateral governance committee is in the process of being established. This includes a Director, Executive Manager, Secretary, Treasurer and Researcher in both Cork and Omdurman. These groups will meet on a regular basis and will work together to ensure the partnership meets all of its legal, financial, administrative, educational and research objectives.
Joint Committee on Foreign Affairs & Trade
The Irish Oireachtas Joint Committee on Foreign Affairs and Trade (JCFAT) has learnt of the significant role the Cork University Maternity Hospital (CUMH) - Omdurman Maternity Hospital (OMH) partnership plays in Northern Sudan. The Committee, chaired by Mr Pat Breen, TD, previously extended an invitation to Univeristy College Cork's Centre for Global Development to present on its work across a diverse range of interlocking global issues. Over 100 staff members at UCC are involved in a range of on-going global development research, teaching and volunteering projects.
The live-streamed and public meeting on Wednesday 24th April 2013 featured an animated discussion between the CGD team and TDs and Senators, with over two dozen questions from Committee members on a range of themes related to the projects, as well as the overall contribution universities, and UCC’s CGD in particular, are making to the complex area of global development.
Professor Tony Ryan, Consultant Neonatologist at CUMH and Professor of Neonatology, Department of Paediatrics and Child Health, UCC presented the Helping Baby Breathe (HBB) project. Funded by Irish Aid Prof Ryan’s colourful presentation used a mannequin of a baby to demonstrate how village midwives can save young lives by focusing on the baby during the first or ‘golden minute’ after birth. He noted that changing birthing practices to ensure a focus on this ‘golden minute’ has led, based on research evidence, to many lives being saved in Sudan where he, together with a colleague, Dr Sami Ahmed (Bons Secours Hopsital, Cork) have been promoting the HBB project (originally developed by the American Academy of Paediatrics) over the last number of years.

The HBB is a basic neonatal resuscitation curriculum specifically developed for resource-limited circumstances. It is based on the premise that assessment at birth and simple new-born care are basic standards that every baby deserves. HBB emphasises skilled attendance at birth, assessment of every baby, temperature support, stimulation to breathe, and assisted ventilation as needed, all within “The Golden Minute” after birth.
The video of Prof. Ryan's presentation to the JCFAT can be viewed here: http://www.youtube.com/watch?v=F2tyqNtGFBc
The vide of Prof. Ryan's Q&A session at the JFCAT can be viewed here: http://www.youtube.com/watch?v=hAvQZcAzxYg
Helping Babies Breathe
Irish Aid, Irish & American Paediatricians and Nurses
and Helping Babies Breathe (HBB) in Sudan
LAUNCH of H.B.B, KHARTOUM, SUDAN - JANAURY 2013
Imagine you are in a remote Sudanese village, a collection of 50 or so, single-story mud houses. The village midwife has been monitoring Salma throughout her pregnancy. She is summoned because Salma is in labour. She picks up her aluminium box, the size of a square overnight case. The equipment inside has already been sterilised by boiling and resealed following the last delivery. She picks up a bucket filled with cooled boiled water, puts on her uniform, a linen white sari, and she waddles over to Selma’s house with her box in one hand and her water bucket in the other. Village people are beginning to gather around the hut. A birth in the village is a festival.
The midwife begins to make arrangements for the delivery. Inside the hut are the mothers of Salma and her husband. This is Salma’s first baby. The midwife washes her hands carefully. She does not have any disposable gloves. Indeed, 80% of babies in Sudan are delivered into midwives’ un-gloved hands. As the labour progresses towards the delivery, the midwife performs an episiotomy, often without local anaesthetic because supplies have run out. Selma is being held down and supported by her grandmothers. She has had no painkillers during her labour. When the baby is born the midwife cuts the cord, hands the baby to the grandmothers and addresses herself to delivering the placenta and suturing the episiotomy. The grandmothers have seen many babies born but they have also seen many babies die, including some of their own. They begin to wash their new grandchild baby who is limp and crying weakly. They put on some fine clothes. They are worried that the baby is not crying and indeed the midwife confirms that the baby has died. The village is saddened, but they are used to this and they say that Selma can have another baby next year, a healthy baby who will survive.
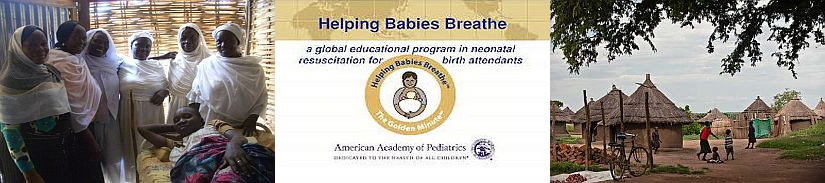
Imagine a year later, Salma is pregnant, about to deliver and the same midwife is called. The midwife has been taught a programme called ‘Helping Babies Breathe’ at the Health Centre many miles away from the village. She has been given a piece of equipment called a bag/mask. She learned to put the mask over the mouth of a baby mannequin and to squeeze the bag so as to pump air into the mannequin’s lungs. She had never before in her life seen one of these devices. She has tended to it carefully, keeping it in a plastic bag to prevent it from contamination and sand.
Salma’s baby is delivered. This time the midwife places the baby on the Salma’s tummy to keep her baby warm. She dries the baby vigorously. She wipes a little fluid from her mouth and stimulates her by rubbing her back. She puts on a dry towel to keep the baby warm. She looks at the baby’s chest. She heard no cry and the baby is not breathing. She immediately cuts the cord, brings the baby over to the table where her bag/mask device was carefully laid out. She suctions the baby’s mouth, puts the mask over the baby’s face, squeezes air into the baby’s lungs. She chants to herself as she had been taught : ‘breathe..2…3, breathe..2…3, breathe..2..3. She continues this for a minute without interruption. She feels the baby beginning to struggle. She takes off the mask and the baby cries. Salma’s second baby has arrived safely into the world by the help of a midwife who learned how to Help Babies Breathe!

In January 2013 a team of doctors and nurses from Ireland, USA and Northern Sudan undertook a week long intensive Master Train the Trainer Helping Babies Breathe programme. The master trainers included;
- Prof Anthony Ryan, Consultant Neonatologist, Cork University Maternity Hospital, Cork, Ireland.
- Dr Sami Ahmed, Consultant Paediatrician, Bons Secours Hospital, Cork, Ireland.
- Dr Abdel Moniem Hamid, Consultant Paediatrician, Khartoum General Hospital, Sudan.
- Prof George A. Little, Co-Chairperson of the HBB Global Implementation Task Force, Department of Paediatrics, Children’s Hospital, Dartmouth-Hitchcock Medical Centre, Lebanon, New Hampshire, USA.
- Dr Carol Little, Department of Paediatrics, Children’s Hospital, Dartmouth-Hitchcock Medical Centre, Lebanon, New Hampshire, USA.
- Dr Lisa Clark, Paediatric Nurse Practitioner at Stony Brook Long Island Children’s Hospital, USA.
- Victoria Flanagan, RN, MS, Regional Program for Women’s and Children’s Health, Dartmouth-Hitchcock Medical Centre, USA.
With a grant from Irish Aid, their aim was to teach village midwives the Helping Babies Breathe Programme, developed by the American Academy of Pediatrics. The philosophy of HBB is simple: it is a plea to the midwife to Give the first minute of life to the baby. Most babies who do not breathe within the first minute of birth will die. Most babies who breathe or who are helped to breathe will survive. Over 4 days, they trained 40 Paediatricians and Senior Health Midwives who then trained 40 Village Midwives from all over Sudan in the Helping Babies Breath Programme. The days were filled with teaching activities, hands-on training, feedback and encouragement.
At the closing ceremony, 1,000 bag-mask devices from Irish Aid were distributed to health care teams from each of the 15 States in Northern Sudan. Each team was committed to teaching other village midwives in their locality. However, there are 14,000 more midwives in Sudan. It costs €80 to train a midwife and provide her with a bag-mask resuscitation device. Can we reach out to them to Help Babies Breathe?
50 Years of Sudanese Obstetric Outcomes
According to the most recent World Health Statistics report from the World Health Organization in 2010, Sudan’s reported maternal mortality ratio (MMR) estimate was 1,107 deaths per 100 000 live births. This is above the African regional estimate of 900 per 100,000 live births, and is significantly higher than the estimated MMR in the European region of 27 per 100,000 live births. Likewise, neonatal mortality in Sudan is significant, at 41 per 1,000 live births, compared with less than ten per 1000 live births in Europe.
Thanks to researchers at Omdurman Maternity Hospital and Cork University Maternity Hospital over 50 years of Sudanese obstetric outcomes were examined and collated toghether for a publication in the British Journal of Obstetrics and Gynaecology (BJOG) in 2011. The paper shows a unique historical portrait of health outcomes in one of the largest maternity hospitals in Africa, and shows steady, sustained improvements in maternal, stillbirth and neonatal mortality rates since the 1990s. The CUMH-OMH partnership was associated with a number of positive infrastructural, educational, and staffing achievements over the last decade and this seminal journal article is a testiment to strength of this partnership.
Reference: Carlson V, Omer M, Ibrahim S, Ahmed S, O’Byrne K, Kenny L, Ryan C. Fifty years of Sudanese hospital-based obstetric outcomes and an international partnership. BJOG 2011;118:1608–1616.
Fifty years of Sudanese hospital-based obstetric outcomes and an international p

UCC's Centre for Global Development - Annual Report 2012
The Cork - Omdurman Partnership Project (COPP), now known as the Cork University Maternity Hospital (CUMH) - Omdurman Maternity Hospital (OMH) Partnership, was included in University College Cork's (UCC) Centre for Global Development Annual Report in 2012 (pages 16-17). The Centre for Global Development (CGD) is the main vehicle for UCC’s global development strategy and is the outward expression and umbrella forum of the wide range of development work which UCC staff, students and personnel are involved with. The Helping Babies Breathe project in Northern Sudan was also included in the CGD Report (page 22-23) which is publicised to a wide international audience and printed and distributed around the world.
The CGD Annual Report for 2012 can be viewed online or downloaded to your computer here: UCC's Centre for Global Development - Annual Report
Sudanese Outstanding Partnership Award
In January 2013, during a week long research and training visit to Khartoum, Northern Sudan, Prof. Anthony Ryan and Dr Sami Ahmed were presented with an Outstanidng Partnership Award by Prof. Mamoun Humaida, Minister of Health for Khartoum State for building up the Cork-Omdurman partnership over the last number of years and for their commitment to improving maternal and child health in Northern Sudan.
Ms Siobhán O’Connor along with Mr Yusuf Malik were also presented with gifts by Dr Murwan Omer, Clinical Director of Omdurman Maternity Hospital for their contribution to education and research at OMH. The awards ceremony at the Coral Hotel, Khartoum concluded with a civic reception and dinner attended by members of the Ministry of Health, the Sudanese Medical Council, the Sudan Association of Paediatricians and the Sudanese Society of Neonatologists.

