Vitamin D

Frequently Asked Questions
Why do we need vitamin D?
Vitamin D is important for healthy bones and good overall health throughout life. Calcium and phosphorous are essential for developing the structure and strength of bones and teeth, and our bodies need vitamin D to absorb these essential minerals. Researchers are now discovering that vitamin D may also be important in helping us to fight infection and in making sure that our muscles, heart, lungs and brain are healthy.
Where do we get vitamin D from?
The main source of vitamin D for humans comes from the action of sunlight on the skin. Cholecalciferol is produced under the skin on exposure to ultraviolet blue (UVB) sunlight. Cholecalcifereol then undergoes a number of chemical changes in the body to produce the active form of vitamin D that can be used by the body.
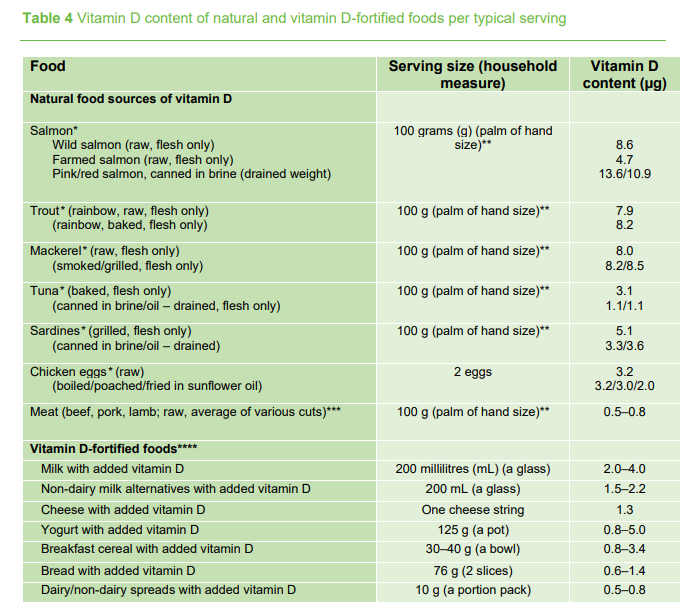
Vitamin D can be also be obtained from foods in the diet, fortified foods and supplements. However, for most people, the amount of vitamin D provided in the diet is low. This is because very few foods contain high levels of vitamin D naturally. Oily fish such as salmon, tuna, and mackerel and fish liver oils are among the best sources of vitamin D but are not commonly eaten. Small amounts of vitamin D are found in meat, dairy foods and eggs. Some foods have vitamin D added, such as certain milks, margarine, breakfast cereals, breads and others, but the foods that are fortified with vitamin D differs by country.
Vitamin D supplements are effective in those who take them, however, supplement use is voluntary and tends to be highest amongst young children and older people and lowest amongst children, teenagers and young adults, who are also at risk of deficiency.
Taken from Report of the Scientific Committee of the Food Safety Authority of Ireland Vitamin D: Scientific Recommendations for 5 to 65 Year Olds Living in Ireland, 2023.
What are the recommended dietary intakes for Vitamin D?
The Institute of Medicine in the United States suggests that the average person needs 10 µg of vitamin D each day. Some people will need as high as 15 to 20 µg of vitamin D. The relevant expert authorities in the UK and Nordic region recommend 10 µg of vitamin D each day. All of these recommended intakes have been established with a view to protecting the bone health of the population.
The ODIN project, which is being co-ordinated by Professors Kiely and Cashman here at the Cork Centre for Vitamin D and Nutrition Research is carrying out research studies to provide the scientific evidence on which to base recommended dietary intake for vitamin D for children, teenagers, pregnant women and dark-skinned ethic groups. These subgroups are covered in the current recommendations but have been based on very limited experimental data up to now.
Is daily sun exposure enough to ensure adequate vitamin D status?
A major source of vitamin D for humans is its production in the skin on exposure to ultraviolet B (UVB) sun light. However, during wintertime in latitudes (distance north or south from the earth’s equator) greater than ∼38°, the strength of UVB light from the sun is too weak to allow for vitamin D to be produced in the skin. This is due to the fact that the angle of the sun is too oblique for UVB rays to pass through ozone, so little or no vitamin D is produced via the action of sunlight on the skin. This “vitamin D winter” increases with latitude; it lasts about 3 months in Athens, Greece (37°N), ∼6 months in Cork, Ireland or London, UK (both at 51°N) and 7–8 months in Helsinki, Finland (at 60°N) and Tromsø, Norway (at 70°N).
Personal behaviour also limits UVB exposure, even in sunny countries. As excessive sun exposure is the principal risk factor for most skin cancers, public education campaigns recommend limiting exposure to sunlight. More people are following the sun safety recommendations and awareness of the links between too much sun exposure and skin cancer, as well as premature wrinkles, has led to the widespread use of sunscreen and inclusion of sun protection factor (SPF) ingredients in cosmetic products. However, it has been shown that correct application of a product containing an SPF of 15 almost completely prevents skin production of vitamin D.
Reduced exposure of the skin to sunlight in the case of individuals who wear clothes that cover more of the body’s skin reduces sun exposure particularly in veiled women. For many people, the long working hours spent indoors mean that they rely on weekends and holidays to spend time outdoors during the day.
People with darker skin are at higher risk of low vitamin D status as they have more melanin in their skin which reduces the ability of UVB rays to penetrate the skin and thus reduces the body’s ability to make vitamin D. Also, as people get older, the body’s ability to produce vitamin D from the sun becomes less efficient due to effect that the ageing process has on the skin.
Thus, there are many reasons why people are unable to get enough daily sun exposure to make adequate amounts of vitamin D. This means that they are dependent on dietary sources to ensure adequate vitamin D status. However, in Ireland and other European countries, natational dietary surveys have shown low dietary intakes of vitamin D; therefore, supplementation and food fortification may be a solution to prevent low vitamin D status.
Is it necessary to give babies a vitamin D supplement?
Yes, the current advice from the Health Service Executive (HSE, 2016) in Ireland is that all babies, regardless of whether they are breastfed, formula fed or taking solids should be given 5 micrograms (5µg) of vitamin D3 daily. Vitamin D is important as during the first year of life babies are growing very quickly and have a high requirement for vitamin D to absorb enough calcium to build strong bones and teeth. In Ireland, studies have shown that children (and adults) in Ireland have low levels of vitamin D which can results in weak bones. In severe cases low levels of vitamin D can result in rickets in children (see next question for more information on Rickets).
Babies’ skin is very sensitive to the sun and should not be exposed to direct sunlight, thus they will not be able to make their own vitamin D from the action of sunlight on the skin. Furthermore, their food (breast milk, formula and solid food) may not have enough vitamin D for to cover their needs. Thus, it is important that babies are given a vitamin D supplement.
Furthermore, babies born to African, Afro-Caribbean, Middle- Eastern or Indian mothers are at even higher risk of having low levels of vitamin D. Their stores of vitamin D may be particularly low when born as their mothers’ skin may not be as efficient at making vitamin D from the amount and type of sunlight in Ireland.
What is rickets? What should I do if I suspect my child has rickets due to vitamin D deficiency?
Rickets is a condition that affects bone development in children. It causes bones to become weak, which can lead to bone deformities. Rickets can cause bone pain, poor growth and deformities of the skeleton, such as bowed legs, curvature of the spine, and thickening of the ankles, wrists and knees. Children with rickets are also more likely to fracture their bones.
It is essential for children to get enough vitamin D so they can absorb calcium to form strong bones and teeth. A lack of vitamin D or calcium is the most common cause of rickets. However, in rare cases, children can be born with a genetic form of rickets. Rickets can also develop if the child has a medical condition that affects the absorption of vitamins and minerals by the body.
Rickets was common in the past, but it almost disappeared in the western world during the 20th century due to better nutrition. However, in recent years there has been in increase in the cases of rickets in Ireland. However, in recent years there has been in increase in the cases of rickets in Ireland. Over the last four to five years, there have been report of up to 20 cases of rickets, among infants and toddlers in two Dublin hospitals.
If a child has any signs or symptoms of rickets, they should be taken to the doctor. The doctor will carry out a physical examination and discuss the child’s medical history, diet, family history or medications. A blood test to measure calcium, phosphorous and vitamin D level may be taken. The doctor may also take an X-ray or possibly a bone density scan (DEXA scan). This is a special type of X-ray that will give the doctor more information about your child’s bones.
What is Osteoporosis? Who is at risk of getting Osteoporosis?
Osteoporosis is the most common bone disease worldwide. In Ireland, it is estimated that 300,000 people suffer from osteoporosis and that one in 4 men and 1 in 2 women over 50 will develop a fracture due to osteoporosis during their life (The Irish Osteoporosis Society, 2016).
Osteoporosis means porous bones and it is often referred to as the silent disease as it is usually not diagnosed until a person suffers from a broken bone or fracture. Bone is a living tissue that is constantly being removed and replaced. Bones need normal sex hormones, calcium, vitamin D, adequate calories, proteins and weight bearing/strengthening exercise to keep them healthy.
As we get older, more bone is naturally lost than is replaced, and people who develop osteoporosis lose more bone than those who do not have the disease. This causes bones to become fragile and therefore they break easily e.g. through a minor bump or fall. A broken bone as a result of a trip or fall from a standing position is not normal at any age. Osteoporosis can affect the whole skeleton, but the most common areas to break are the wrist, spine and hip. The disease affects all age groups and both sexes - it is not just a female or old person’s disease. If you have one fragility (low trauma) fracture, this doubles your risk of another fracture due to Osteoporosis.
Osteoporosis can be prevented in most cases, and is a treatable disease in the majority of people. It is important to be diagnosed as early as possible for the best outcome. A DEXA scan of your spine and hip area is the gold standard for diagnosing Osteoporosis and is highly recommended if you are at risk.
Should vitamin D supplementation be recommended in elderly adults?
Sunlight is a major source of vitamin D; however, since Ireland is situated between latitude 51 and 55 ºN, negligible cutaneous synthesis of vitamin D occurs between October and March. In addition, cutaneous synthesis of vitamin D decreases with age. The Food and Nutrition Board, Institute of Medicine (1997) suggests a daily vitamin D intake of 10µg for adults aged 51-70 years. A recent Irish study found that 89% of 51-64 year olds do not achieve the 10µg/day recommendation, with mean daily intakes (MDI) of vitamin D from food sources being 4.01 µg in men and 3.39 µg in women (Hill et al., 2004). Results from other studies (Hill et al., 2002, 3003) observed low vitamin D status in 50-75 year old Irish women between late winter and early spring. These findings indicate that dietary intake of vitamin D is not sufficient in Ireland to reach recommendations for the elderly population and vitamin D supplementation should be promoted among this population group. Nonetheless, in 2011, the FSAI proposed that all Irish citizens should be taking a daily vitamin D supplement as neither the dietary sources consumed or sun exposure obtained in summer is sufficient to maintain adequate vitamin D status throughout the winter months.
